If you’ve been diagnosed with keratoconus or have a family member with this condition, you might wonder whether your children or other relatives face a higher risk. It’s natural to have concerns about passing on vision problems to the next generation.
Understanding keratoconus, its causes, and when to seek professional care through specialized keratoconus management can help you make informed decisions about your family’s eye health.
Keratoconus does have a genetic component, but it’s not a simple inheritance pattern. Most people with keratoconus don’t have affected family members, and having a genetic predisposition doesn’t guarantee you’ll develop the condition.
What Is Keratoconus and How Does It Start?
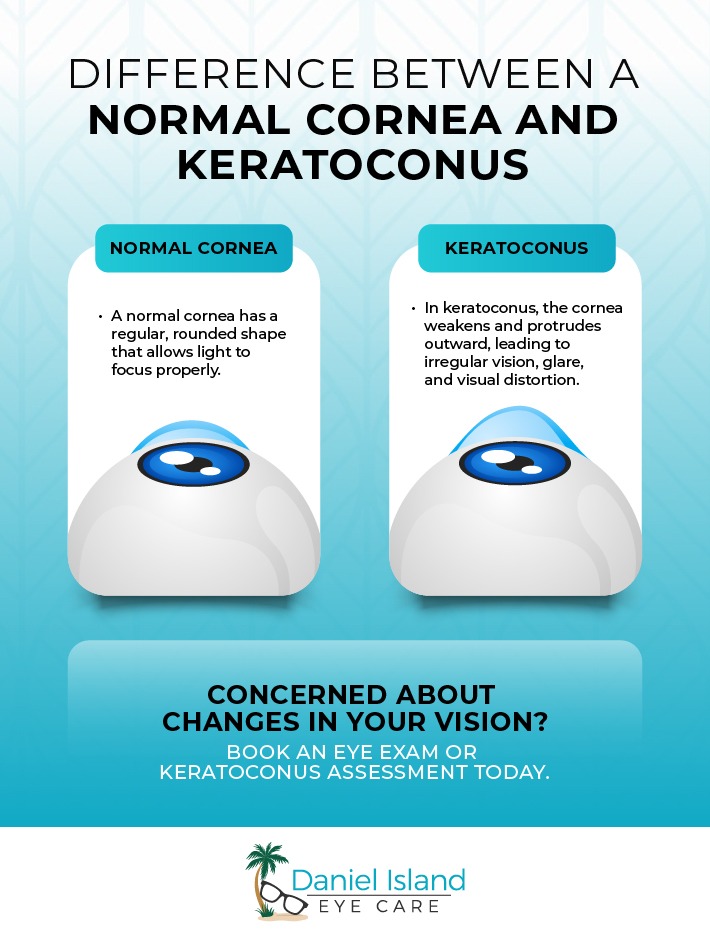
Keratoconus happens when your cornea—the clear front surface of your eye—gradually thins and bulges into a cone-like shape. This irregular shape prevents light from focusing properly on your retina, leading to vision problems.
The condition typically begins during your teens or early twenties and can progress for 10–20 years before stabilizing. You might notice these warning signs:
- Blurred or distorted vision
- Light sensitivity and glare problems
- Frequent prescription changes
- Sudden vision changes
Understanding the 4 stages of keratoconus can help you recognize how the condition progresses from mild to severe over time.
The Genetic Connection: Family History and Keratoconus
Research shows that genetics play a role in keratoconus development, but it’s more complex than a typical inherited condition. Scientists have identified several genetic variations that can increase your risk, but these variations alone don’t cause keratoconus.
About 1 in 10 people with keratoconus have a parent or sibling with the condition. This means your risk increases if you have an affected family member, but it’s still relatively uncommon.
Most people with keratoconus don’t have obvious family connections to the condition. This happens because the genetic factors involved are complex and may skip generations or require specific combinations to become active.
Related Genetic Conditions
Certain genetic conditions can increase your likelihood of developing keratoconus, including:
- Down syndrome
- Ehlers-Danlos syndrome
- Marfan syndrome
- Connective tissue disorders
Environmental Factors That Can Trigger Keratoconus
Even if you carry genetic variants that increase keratoconus risk, environmental factors typically need to combine with your genetic predisposition for the condition to develop. Think of genetics as setting the stage, while environmental factors influence whether the condition appears.
Eye Rubbing and Trauma
Frequent or vigorous eye rubbing can weaken your corneal tissue over time. The mechanical stress from rubbing puts pressure on an already vulnerable cornea in people with genetic predispositions.
Sometimes eye rubbing results from early keratoconus symptoms rather than causing them. You might rub your eyes because they feel irritated or uncomfortable due to vision changes you haven’t noticed yet.
Allergies and Eye Irritation
Allergic conditions such as hay fever, eczema, or asthma often co-occur with keratoconus. These conditions can make your eyes itchy and uncomfortable, leading to more frequent eye rubbing. Allergies can also cause blurry vision, making it even more important to manage these conditions effectively.
Managing your allergies effectively can help reduce eye irritation and the urge to rub your eyes, potentially slowing keratoconus progression if you’re already affected.
Your Risk Factors and What They Mean
Keratoconus typically requires both genetic susceptibility and environmental triggers to develop. Having one or even several risk factors doesn’t mean you’ll definitely develop the condition.
Your personal risk depends on multiple factors working together—family history, genetic variations, eye rubbing habits, allergic conditions, and possibly other factors we don’t fully understand yet. This complexity explains why predicting who will develop keratoconus remains challenging.
Many people carry genetic variants associated with keratoconus but never develop symptoms. Your genes might make you more susceptible, but your lifestyle and environment also play important roles in whether the condition actually appears. It’s worth noting that while some people worry about keratoconus causing blindness, complete vision loss from this condition is extremely rare with proper management.
When to Seek Eye Care
If you have family members with keratoconus or notice vision changes, schedule a comprehensive eye exam. Early detection can help us monitor your condition and start treatment sooner if needed.
Catching keratoconus early matters because we have treatments that can slow its progression. The sooner we identify changes in your cornea, the more options we have to help preserve your vision.
Regular comprehensive eye exams can detect keratoconus before you notice symptoms. We use modern diagnostic technology to measure your corneal shape and thickness, identifying subtle changes that might indicate early keratoconus.
Treatment options range from glasses and soft contact lenses for mild cases to specialized scleral lenses for more advanced keratoconus. We can also discuss procedures that help strengthen your cornea and slow progression when appropriate.
Keratoconus Care Starts Here
At Daniel Island Eye Care, we have extensive experience managing keratoconus and helping patients maintain clear, comfortable vision. If you have concerns about keratoconus risk or symptoms, contact us to schedule your comprehensive eye exam and discuss your family history and personal risk factors.